Trigger finger

Trigger finger is a common condition and is a narrowing of a
portion of the tendon sheath in the finger (or thumb) that interferes with normal finger movement. This condition is most common in the ring finger but can affect any finger. It is more common in middle aged women, but also occurs in the very young especially in the thumb. It is called trigger finger because of the characteristic resistance to movement followed by a sudden release, which mimics the action of a trigger on a gun.
What is trigger finger?
As the finger is bent and extended the fingers flexor tendon glides smoothly through a series of pulleys which form a tunnel in the finger of the hand. Trigger digits results from a narrowing of one of the tunnels; called the first annular or A1 pulley. Repeated movement of the tendon through the tight tunnel causes the tendon to swell and some of the tendon fibres can become worn and torn. As a result the tendon can swell and thicken, forming a nodule. Because of the inflammation and scarring which occurs the pulley also thickens and narrows. The swollen tendon or nodule now has trouble passing through the narrow pulley and it gets stuck. With concerted effort or with the help of the other hand this can be overcome and the tendon nodule suddenly passes through the tight tunnel and causes the triggering.
Why have I got trigger finger?
This condition may be caused by over-use or by 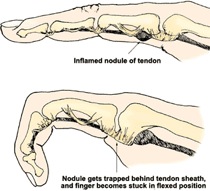
repetitive use of the hand. Several medical conditions can increase a person's risk of trigger digit, including diabetes, rheumatoid arthritis, gout, renal disease and other inflammatory conditions. In rare instances trigger digit can also result from direct trauma over the A1 pulley.
The first symptom is typically a mild sticking sensation at the base of the finger when the finger is flexed or extended. This may be accompanied by pain. A bump may be felt beneath the skin of the palm at the base of the affected finger. The finger may be difficult to extend, and may flick more and catch as it is extended. Typically the patient wakes up in the morning, unable to straighten the finger from the flexed position. This triggering may become severe and if left untreated, the finger can become
locked in the flexed position. Stiffness of the finger may also
develop in cases which are long standing.
What are the none operative treatments?
Anti-inflammatory tablets can be helpful in early cases where there is pain and swelling, but the results are unpredictable. A steroid injection to the flexor tendon sheath has a high success rate of 70%. Patients with Diabetes or rheumatoid arthritis may have less success with steroid injections. If an injection fails to give long term relief of symptoms the next step is surgical release of the pulley. Hand therapy may be necessary after surgery or if finger stiffness is present.
What are the surgical options?
A trigger finger isn't a dangerous condition, so the decision whether to proceed with surgery is a personal one based on the severity of your symptoms. This is a small operation performed under local anaesthetic. A small amount of local anaesthetic is injected into the hand to make it completely numb. A small incision in the palm of the hand, exposes the Pulley which is trapping the tendon. The pulley is released allowing the tendon to slide up and down freely. The incision is closed with an absorbable suture.
What can I expect after surgery?
A bandage is applied to keep the wound clean and limit use of the hand for 5 days after surgery. During this time the hand should be kept above the hart to limit swelling and the fingers should be regularly put through a full range of motion to prevent stiffness. After 5 days the large dressing can be removed leaving the sticky dressing in place, this can be replaced if it gets dirty of loose. At 2 weeks the sticky dressing can be removed and the wound can now get wet and normal use of the hand can be resumed. It will take several weeks for the wound to settle completely. If the finger is stiff physiotherapy may be required.
Return to work, driving and sports?
Sedentary office type work can be resumed immediately. It will normally be 2-3 weeks before it is safe to return to heavy manual work. Return to driving after the bulky dressing is removed at 5 days.